PrEP DAP eligibility and services can change. Please call for information at 360-236-3412 or 877-376-9316 (toll free) or email at PrEPDAP@doh.wa.gov.
PrEP DAP Provider Contract
Client Services EIP and PrEP DAP Provider Contract (PDF)
Medical and Lab Services
PrEP DAP pays for limited PrEP-related medical visits and lab tests.
Enrollees must go to providers and labs that contract with PrEP DAP.
For Enrollees with insurance, PrEP DAP covers the patient portion of insurance deductibles, copays, and coinsurance, up to the maximum amount listed on our list of covered services.
For Enrollees without insurance, we pay full cost, up to the maximum amount listed on our list of covered services.
What Medical & Lab Services are Covered?
Current list of medical and lab services and the maximum amount PrEP DAP covers for these services: PrEP DAP List of Covered Services (PDF)
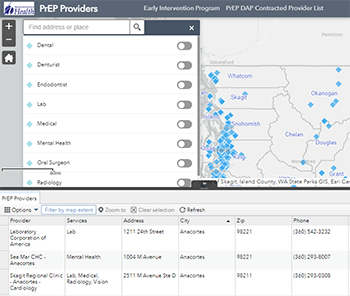
Provider Locator
Enrollees must be seen by a PrEP DAP Contracted Provider (Both Medical Provider and Lab) in order for the claim to be paid by PrEP DAP. Enrollees can find a PrEP DAP provider or lab using our interactive map below.
Disclaimer: When selecting a contracted provider office, keep in mind there is no guarantee they are accepting new patients. Contact the provider office or lab you select to check availability and type of insurance accepted. New providers will be added often so check back for updates.
Interactive provider map and list of contracted providers
-
Select contracted providers map link or click on map image below
-
After you select the "Go" button, you can use the search box above the map to select the type of care you need.
- The map will display locations of providers for the type of care you chose.
- You will also see a list beneath the map with name, type of service, location and contact information.
- Complete list of contracted providers (PDF)
- Complete list of contracted providers (XLSX)
What do I do if I receive a medical bill?
For enrollees with insurance, we have provided below a Frequently Asked Questions (FAQ) about Medical Bills for enrollees with insurance about what to do if you receive a bill:
FAQ about medical bills - instructions for clients with insurance (PDF)
For enrollees who do not have insurance, being enrolled in PrEP DAP means we pay your portion of the claim. We pay the maximum amount allowed for services we cover. Contracted providers are not allowed to bill enrollees for covered services. Sometimes it happens. If it does and you receive a bill, contact our office so we can work with your provider to resolve the issue.
Having Issues with your Provider or Insurance Plan?
Provider Complaints
Please read the frequently asked questions (FAQ) before completing the complaint form, as you may be able to resolve your issue from the responses posted. If the FAQ does not resolve your issue, submit an online complaint by using the Health Systems Quality Assurance Complaint Intake Form.
Insurance Company or Plan Complaints
Complaints about an insurance company or plan are handled through the Office of the Insurance Commissioner (OIC). Submit your complaint on the OIC website
Need Help Appealing an Insurance Denial or Policy Decision?
There is help available. Insurance plans are required to notify consumers of appeal rights and consumer protection services available to them when a negative action is taken against a policyholder. A negative action can include a claim denial, benefit denial, reduced payment or policy cancellation. More about appealing a health insurance denial
